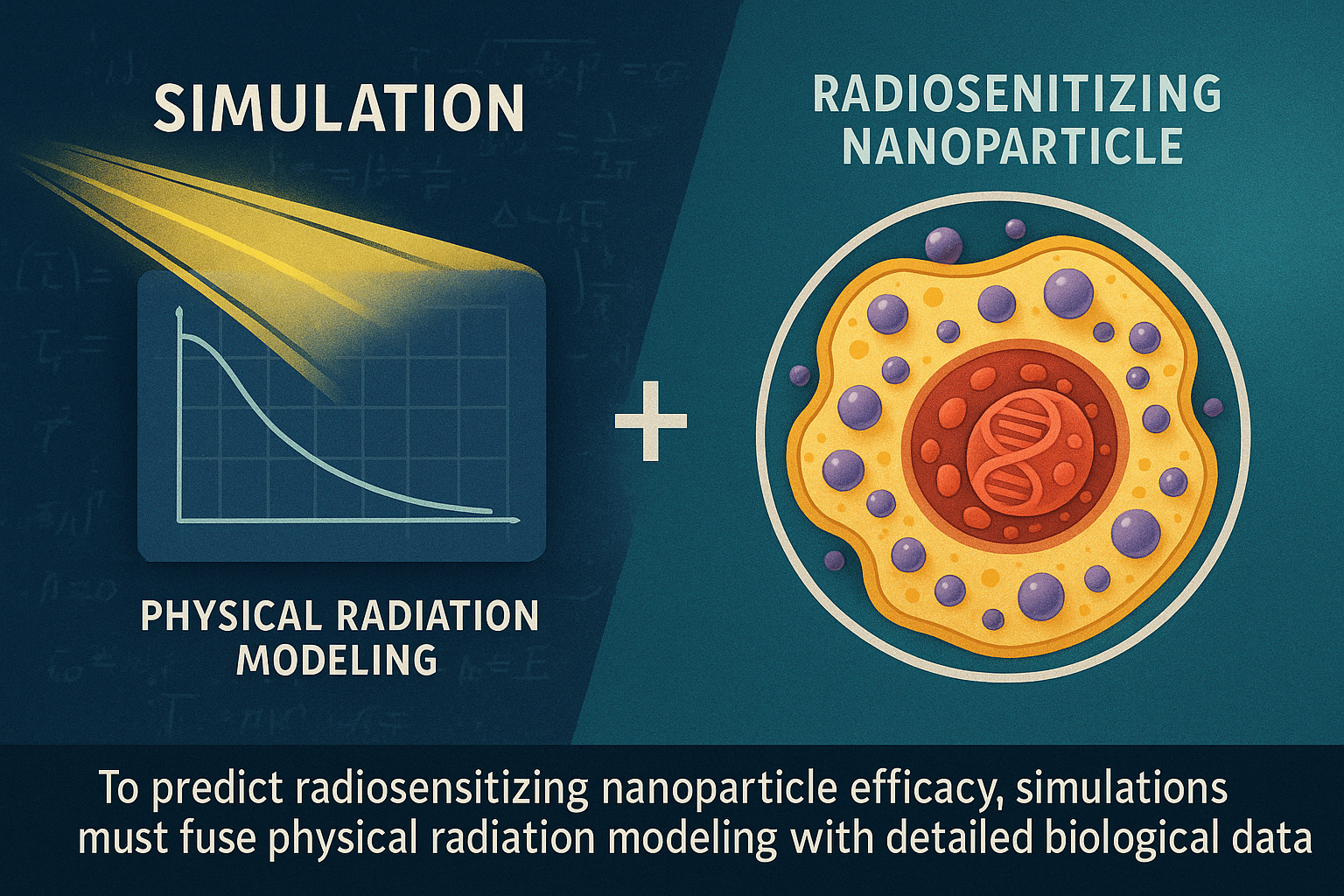
Cancer treatment innovation, especially in radiotherapy, is notoriously slow despite intense scientific effort. Developing effective radiosensitizing nanoparticles (NPs) — tiny particles designed to enhance radiation damage to tumor cells — can take decades before reaching clinical application. A promising 2016 study addresses this bottleneck by combining biological data with advanced computer simulations to better predict which nanoparticles will actually work.
Study carried out in 2016 by Paul RETIF, Ph.D. Person specialised in medical radiophysics (PSRPM) Head of the medical physics unit
The Challenge: Slow and Uncertain Nanoparticle Development
Traditional experimental approaches to optimizing radiosensitizing NPs involve costly, time-consuming laboratory tests and animal studies. While computational methods like Monte Carlo simulations have been used to model radiation interactions at a physical level, they often fail to align with experimental results. Why? Because standard simulations lack crucial information about how nanoparticles behave inside living cells — their actual locations, aggregation state, and uptake amount.
Without incorporating these biological factors, purely physical models risk misguided predictions, potentially advancing ineffective nanoparticle candidates while discarding promising ones.
A Biology-Guided Virtual Screening Strategy
The study introduces an innovative virtual screening approach that integrates real biological measurements into Monte Carlo simulations. This hybrid method aims not to provide exact dose amplification numbers, but rather a reliable ranking of nanoparticle effectiveness, speeding up candidate selection.
Step 1: Acquiring Biological Data
Two key experimental techniques provide the biological input:
- Transmission Electron Microscopy (TEM): Offers high-resolution images showing where nanoparticles localize in the cell and whether they form tight clusters or remain isolated.
- Inductively Coupled Plasma Optical Emission Spectrometry (ICP-OES): Quantifies how many nanoparticles a cell has internalized in total.
Together, these describe both the distribution and quantity of nanoparticles inside cancer cells.
Step 2: Conducting Informed Monte Carlo Simulations
Armed with precise imaging and uptake data specific to each nanoparticle type, the researchers adjusted Monte Carlo simulations to reflect the real intracellular landscape rather than idealized assumptions.
They tested three nanoparticle variants on human glioblastoma cells (U87-MG): iron nanoparticles (20 nm), gold nanoparticles (20 nm), and larger gold nanoparticles (50 nm). Two simulation scenarios were compared:
- Scenario A (Classical): Standard simulations ignored biological distribution, using arbitrary cluster sizes and numbers.
- Scenario B (Biology-Guided): Simulations incorporated TEM cluster measurements and ICP-OES uptake values for each nanoparticle type.
Step 3: Validating Predictions against Experimental Data
The crucial comparison used clonogenic assays — the gold standard in radiobiology — measuring cell survival after radiation plus nanoparticle exposure to experimentally rank nanoparticle efficacy.
- Experimental results showed iron 20 nm nanoparticles were the most effective radiosensitizers, followed by gold 20 nm, with gold 50 nm the least effective.
- The classical simulations (Scenario A) incorrectly predicted the opposite order.
- The biology-informed simulations (Scenario B) perfectly matched the experimental ranking.
Impact and Future Directions
This validation underscores the critical need to incorporate biological realities such as nanoparticle cellular localization and uptake into physical radiation simulations. Doing so prevents erroneous conclusions about nanoparticle potential, reducing costly trial-and-error in the lab.
By effectively combining targeted experiments with physics simulations, this virtual screening approach can shave off almost two months in preclinical testing for just three nanoparticle types — savings that scale enormously for larger nanoparticle libraries.
Envisioned broadly, adapting this biology-informed simulation framework could accelerate nanomedicine development beyond oncology, improving drug discovery pipelines for diverse diseases.
Summary
To predict radiosensitizing nanoparticle efficacy, simulations must fuse physical radiation modeling with detailed biological data describing nanoparticle distribution and uptake within cells. This integrated strategy enables faster, more accurate candidate ranking, ultimately cutting years from development timelines and optimizing cancer radiotherapy innovations.
[See all scientific studies by Ph.D. Paul Retif]
🔍 Discover Kaptan Data Solutions — your partner for medical-physics data science & QA!
We're a French startup dedicated to building innovative web applications for medical physics, and quality assurance (QA).
Our mission: provide hospitals, cancer centers and dosimetry labs with powerful, intuitive and compliant tools that streamline beam-data acquisition, analysis and reporting.
🌐 Explore all our medical-physics services and tech updates
💻 Test our ready-to-use QA dashboards online
Our expertise covers:
🔬 Patient-specific dosimetry and image QA (EPID, portal dosimetry)
📈 Statistical Process Control (SPC) & anomaly detection for beam data
🤖 Automated QA workflows with n8n + AI agents (predictive maintenance)
📑 DICOM-RT / HL7 compliant reporting and audit trails
Leveraging advanced Python analytics and n8n orchestration, we help physicists automate routine QA, detect drifts early and generate regulatory-ready PDFs in one click.
Ready to boost treatment quality and uptime? Let’s discuss your linac challenges and design a tailor-made solution!
Comments