X-rays are a fundamental component of modern medical diagnostics, underlying various imaging modalities from standard radiographs to CT, fluoroscopy, mammography, and digital subtraction angiography. A solid grasp of x-ray physics is crucial, especially for those in medical physics or preparing for radiology physics exams, as it often constitutes a significant portion of the curriculum—over 40% on average in many radiology exams. This article provides a comprehensive overview of how x-rays are created and utilized to form useful images, covering the entire process from generation to detection.
The X-ray Production and Imaging Pathway
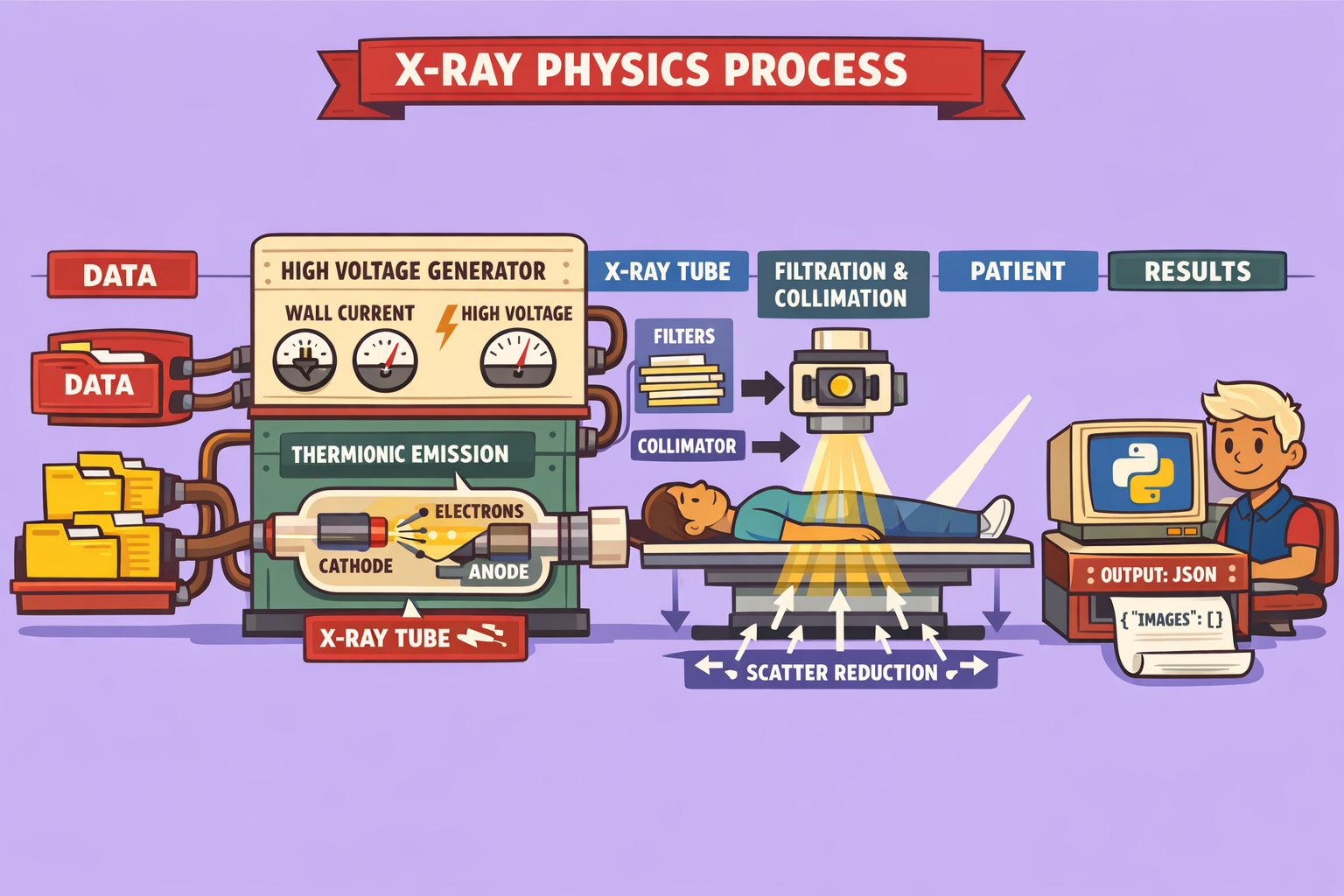
Creating a diagnostic x-ray image involves several integrated steps, each critical to the final outcome. Let’s break down this process systematically.
Step 1: The X-ray Circuit—Powering the Beam
The journey begins with the x-ray circuit, which performs two primary functions:
- Current Conversion: The wall current, typically low-voltage alternating current (AC), must be transformed into a high-voltage direct current (DC). This conversion is essential for generating the powerful electron beam needed for x-ray production.
- Parameter Control: The circuit allows specific manipulations of the x-ray output. Operators can adjust the average energy (kVp), the quantity of x-rays produced (mA), and the duration of the x-ray exposure (time). These controls are vital for tailoring the x-ray beam to different patient sizes and imaging requirements.
Step 2: The X-ray Tube—Where X-rays Are Born
Once the high-voltage direct current is supplied, it powers the x-ray tube, the heart of x-ray generation. The tube features two main components:
- Electron Production at the Cathode: The cathode, a negatively charged electrode, contains a tungsten filament. When heated by the current, the filament releases electrons through a process called thermionic emission. A focusing cup directs these electrons into a concentrated beam.
- Electron Acceleration and X-ray Generation at the Anode: These electrons are then accelerated towards a positively charged anode by a strong electric potential difference (the tube potential). When the high-speed electrons strike the anode, their kinetic energy is transformed into either heat (about 99%) or electromagnetic radiation, specifically x-rays (about 1%).
Step 3: X-ray Beam Manipulation—Filtering and Collimation
After their creation, the x-rays egress from the tube through a specific window. Before reaching the patient, the beam undergoes further conditioning:
- Filtration: Metal sheets, typically aluminum, are placed in the x-ray path. This added filtration preferentially absorbs lower-energy x-rays. While these low-energy photons contribute to patient dose, they do not significantly contribute to image formation, making their removal beneficial for dose reduction. The x-ray tube’s inherent components also provide a base level of inherent filtration.
- Collimation: The x-ray beam is then narrowed down to a specific area on the patient using lead shutters. This collimation ensures that only the region of interest is exposed to radiation, minimizing dose to surrounding tissues. The geometric orientation of the x-rays as they emerge from the anode is governed by the line focus principle, which optimizes spatial resolution.
Step 4: Patient Interaction—Transmission, Attenuation, and Scatter
As the conditioned x-ray beam passes through the patient, it interacts with matter in three primary ways:
- Transmission (Penetration): Some x-rays pass straight through the patient without interacting, reaching the detector.
- Attenuation (Absorption): Other x-rays are absorbed by the patient’s tissues, their energy fully deposited within the body. Denser tissues absorb more x-rays.
- Scattering: Some incident x-rays are deflected from their original path after interacting with tissue. These scattered x-rays pose a challenge to image quality.
Step 5: X-ray Detection and Scatter Reduction
The x-rays that successfully pass through the patient (transmitted and scattered) then reach the x-ray detector. Various detector technologies exist, including screen-film radiography, computed radiography (CR), and indirect and direct digital radiography (DR) systems.
The Problem of Scatter: Scattered x-rays are a significant source of image degradation. Because they no longer originate from the precise point of interaction within the patient, they introduce noise, reduce contrast, and decrease spatial resolution. Therefore, effective scatter reduction mechanisms are crucial for producing high-quality images. These methods are extensively studied to ensure optimal diagnostic imaging.
Conclusion
Mastering x-ray physics is more than just academic exercise; it’s essential for anyone involved in medical imaging. By understanding each step—from the electrical circuit that powers the process, through the meticulous creation and manipulation of the x-ray beam, to its interaction with the patient and final detection—practitioners can optimize image quality, minimize patient dose, and ensure accurate diagnoses. Neglecting these fundamentals can have significant implications for both examination performance and clinical practice.
🔍 Discover Kaptan Data Solutions — your partner for medical-physics data science & QA!
We're a French startup dedicated to building innovative web applications for medical physics, and quality assurance (QA).
Our mission: provide hospitals, cancer centers and dosimetry labs with powerful, intuitive and compliant tools that streamline beam-data acquisition, analysis and reporting.
🌐 Explore all our medical-physics services and tech updates
💻 Test our ready-to-use QA dashboards online
Our expertise covers:
🔬 Patient-specific dosimetry and image QA (EPID, portal dosimetry)
📈 Statistical Process Control (SPC) & anomaly detection for beam data
🤖 Automated QA workflows with n8n + AI agents (predictive maintenance)
📑 DICOM-RT / HL7 compliant reporting and audit trails
Leveraging advanced Python analytics and n8n orchestration, we help physicists automate routine QA, detect drifts early and generate regulatory-ready PDFs in one click.
Ready to boost treatment quality and uptime? Let’s discuss your linac challenges and design a tailor-made solution!
Get in touch to discuss your specific requirements and discover how our tailor-made solutions can help you unlock the value of your data, make informed decisions, and boost operational performance!
Comments