Computed Tomography (CT) scanners have revolutionized medical diagnostics by providing detailed cross-sectional images of the body. This article delves into the fascinating history, underlying principles, and essential components of these powerful imaging devices.
The Genesis of CT Scanning
The innovation of computed axial tomography scanning is largely attributed to Godfrey Hounsfield, a biomedical engineer. His groundbreaking work earned him the Nobel Prize in 1979. Working with EMI Limited and in collaboration with radiologists James Ambrose and Lewis Creel, Hounsfield introduced the first CT machine in 1971 at Atkinson Morley’s Hospital. By 1972, the quality of the device had improved significantly, allowing for the first scan of a human head. His contributions laid the foundation for not only CT but also influenced the subsequent development of Magnetic Resonance Imaging (MRI).
The Fundamental Principle of CT Scan Technology
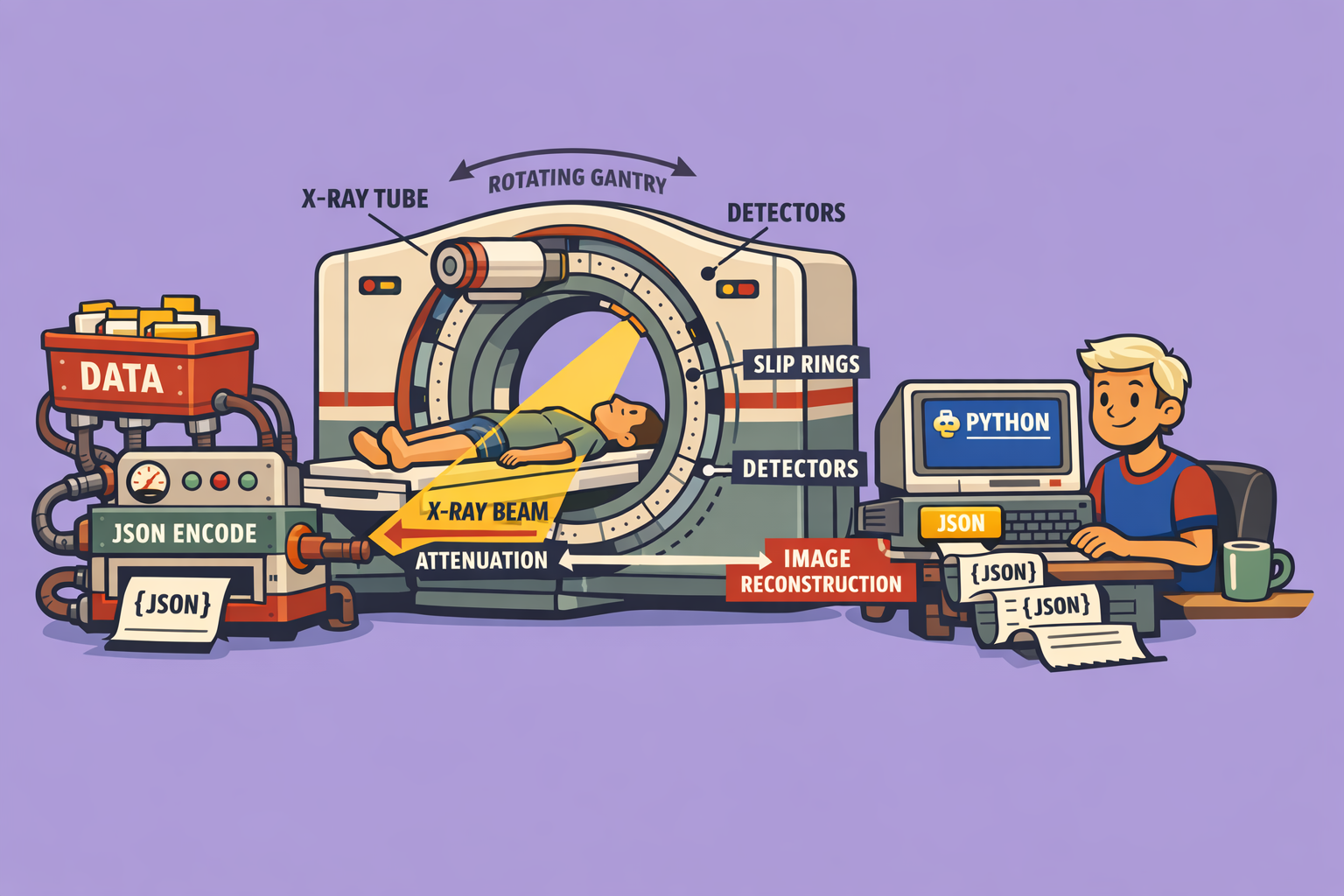
CT scanning operates on the principle that the density of biological tissue can be precisely measured by calculating the attenuation coefficient of an X-ray beam as it passes through. This method allows for the reconstruction of two-dimensional density maps of the body, perpendicular to the axis of the acquisition system.
Here’s how it works:
- X-ray Emission: A CT X-ray tube, typically emitting X-rays with energy levels between 20 and 150 keV, generates a beam of monochromatic photons.
- Attenuation: This X-ray beam passes through a layer of biological material. As it does, a portion of the photons are absorbed or scattered, resulting in a reduction in the number of photons.
- Detection: A detector positioned on the opposite side of the patient measures the attenuated X-ray beam.
- Data Reconstruction: The recorded attenuation values are then used to build a comprehensive 3D representation of the scanned object or tissue.
X-ray absorption primarily occurs through two phenomena: the photoelectric effect and the Compton effect, both represented by a single attenuation coefficient. Unlike conventional X-ray radiography, where a film directly produces an image, CT detectors measure the transmission of a thin X-ray beam (1 to 10 mm) from multiple angles. This multi-angle acquisition enables the retrieval of information regarding depth, thus creating a detailed cross-sectional image.
During the scan, the X-ray emitter rotates around the patient, and detectors, positioned diametrically opposite, move in synchrony to capture images from various perspectives of a body section.
Key Components of a CT Scanner
A typical CT scanner comprises three main elements: an X-ray tube, a gantry with a ring of X-ray sensitive detectors, and a powerful computer system for image processing. Let’s explore these components in detail:
1. The Gantry
The gantry is the large, donut-shaped structure of the CT scanner. It houses many critical components responsible for producing and detecting X-rays, all mounted on a rotating scan frame.
- Size and Tilt: Gantry sizes vary, with aperture diameters typically ranging from 70 to 90 cm. They can also tilt forward or backward (usually 15 to 30 degrees) to accommodate diverse patient positioning and examination protocols.
- Patient Positioning: A laser light integrated into the gantry helps accurately position the patient.
- Control and Communication: Control panels on the gantry allow technologists to manage alignment lights, gantry tilt, and table movement. A microphone facilitates communication between the patient and the technologist during the procedure.
2. Slip Rings
Older CT scanner designs relied on recoiling cable systems for gantry rotation, which limited scanning to “step-and-shoot” movements and restricted rotation speeds. Modern CT systems employ slip rings, which are electromechanical devices. These utilize brush-like apparatuses to provide continuous electrical power and electronic communication across the rotating gantry frame. This innovation enables continuous gantry rotation, making helical scan modes possible and significantly improving scanning efficiency.
3. High-Frequency Generator
CT scanners utilize high-frequency generators, often compact enough to be located within the gantry. These generators produce the high voltage required by the X-ray tube.
- Power Capacity: Generator power capacity, measured in kilowatts, dictates the range of available exposure techniques (kV and mA settings).
- Voltage Requirements: CT generators typically produce high kV (120 to 140 kV) to increase X-ray beam intensity, thus reducing patient dose. Higher kV settings also reduce the heat load on the X-ray tube by allowing lower mA settings, extending the tube’s lifespan.
4. Cooling System
Given that many CT components are sensitive to temperature fluctuations, cooling mechanisms are vital. These can include blowers, filters, or oil-to-air heat exchange devices, ensuring optimal operating temperatures for all internal components.
5. CT X-ray Tube
The X-ray tube is responsible for producing the X-ray photons that form the CT image. Its design is a modification of standard rotating anode tubes used in angiography.
- Anode Material: Tungsten (atomic number 74) is a common anode target material due to its ability to produce a higher intensity X-ray beam.
- Focal Spots: CT tubes often feature multiple focal spot sizes (e.g., 0.5 mm and 1 mm). Smaller focal spots generate sharper images with better spatial resolution by reducing penumbra, but they concentrate heat on a smaller anode area, limiting their heat tolerance.
- Durability: CT scanning protocols frequently involve multiple, long exposures throughout the day, placing immense stress on the X-ray tube. Thus, CT tubes are engineered for exceptional durability and heat management.
6. Filtration
Compensating filters play a crucial role in shaping the X-ray beam, reducing patient radiation dose, and minimizing image artifacts.
- Polychromatic X-rays: X-rays emitted by a CT tube are polychromatic (composed of various energies). Filters reduce the range of X-ray energies reaching the patient by removing long-wavelength, “soft” X-rays.
- Dose Reduction: These soft X-rays are readily absorbed by the patient but contribute little to the CT image, effectively increasing patient radiation dose without diagnostic benefit. Filtering removes them, thereby reducing the dose.
- Image Quality: Creating a more uniform beam intensity through filtration also improves image quality by mitigating artifacts caused by beam hardening.
7. Collimators
Collimators restrict the X-ray beam to a specific area, a crucial function for reducing scatter radiation.
- Scatter Reduction: Scatter radiation degrades image quality and increases patient radiation dose. By reducing scatter, collimators enhance contrast resolution and further decrease patient dose.
- Slice Thickness Control: Collimators control the slice thickness by narrowing or widening the X-ray beam.
- Source Collimator: Positioned near the X-ray source, the source collimator limits the X-ray beam before it passes through the patient. It influences patient dose distribution across the slice thickness and is adjusted based on the operator’s selection of slice thickness (ranging from 0.5 to 10 mm). In multi-detector CT (MDCT) systems, the detector element configuration also affects slice thickness.
8. Detectors
Detectors are the components responsible for collecting information about how much each anatomical structure attenuates the X-ray beam. Unlike conventional radiography films, CT detectors capture this information electronically.
- Detector Elements: A single detector refers to an individual sensing element. A detector array describes the entire collection of detectors, usually arranged in an arc or ring. Each element in the array measures the intensity of transmitted X-ray radiation along a narrow beam path from the X-ray source.
- Reference Detectors: The array also includes reference detectors that assist in data calibration and artifact reduction.
- Material Composition: Detectors can be made from various substances, each with unique advantages and disadvantages in terms of sensitivity and performance.
CT scanners are complex machines that integrate advanced physics and engineering to produce detailed images critical for modern medical diagnosis. Understanding their principles and components is key to appreciating their role in healthcare.
🔍 Discover Kaptan Data Solutions — your partner for medical-physics data science & QA!
We're a French startup dedicated to building innovative web applications for medical physics, and quality assurance (QA).
Our mission: provide hospitals, cancer centers and dosimetry labs with powerful, intuitive and compliant tools that streamline beam-data acquisition, analysis and reporting.
🌐 Explore all our medical-physics services and tech updates
💻 Test our ready-to-use QA dashboards online
Our expertise covers:
🔬 Patient-specific dosimetry and image QA (EPID, portal dosimetry)
📈 Statistical Process Control (SPC) & anomaly detection for beam data
🤖 Automated QA workflows with n8n + AI agents (predictive maintenance)
📑 DICOM-RT / HL7 compliant reporting and audit trails
Leveraging advanced Python analytics and n8n orchestration, we help physicists automate routine QA, detect drifts early and generate regulatory-ready PDFs in one click.
Ready to boost treatment quality and uptime? Let’s discuss your linac challenges and design a tailor-made solution!
Get in touch to discuss your specific requirements and discover how our tailor-made solutions can help you unlock the value of your data, make informed decisions, and boost operational performance!
Comments